35 medicare appeal process diagram
Reopenings are separate from the appeals process, and therefore, do not count towards the five levels of appeal. Note: Reopenings (TOB XXQ) cannot be submitted with a hardcopy (paper) UB-04. They must be submitted via the 5010 format or entered directly into the Fiscal Intermediary Standard System (FISS) via Direct Data Entry (DDE). If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
How to file an appeal if your Medicare Advantage Plan doesn't cover an item or service If you have a Medicare Advantage Plan, you know it covers a lot of items and services, like prescription drugs, diabetic test supplies, cardiovascular screenings, and hospital visits.

Medicare appeal process diagram
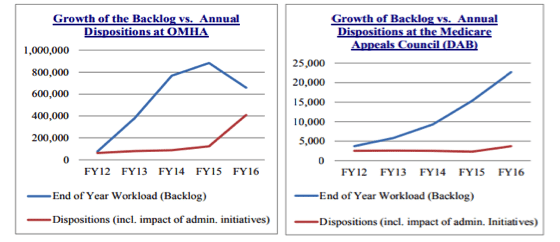
Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review. Medicare Hearin gs and A ppeals ALJ Hearing AIC ≥ $180** No statutory time limit for processing . Medicare Appeals Council . No statutory time limit for processing . F. ederal District Court AIC ≥ $ Review1,760** First Appeal . Level Second Appeal Level Third Appeal Level Fourth Appeal Level Judicial A third level appeal is a bit more interesting as it requires the hearing to be held over the phone, and at times may require a video teleconference; although extremely rare, it may even be in person. Fourth level of appeal . Fourth level appeals are reviewed by the Medicare Appeals Council within the Department of Health & Human Services.
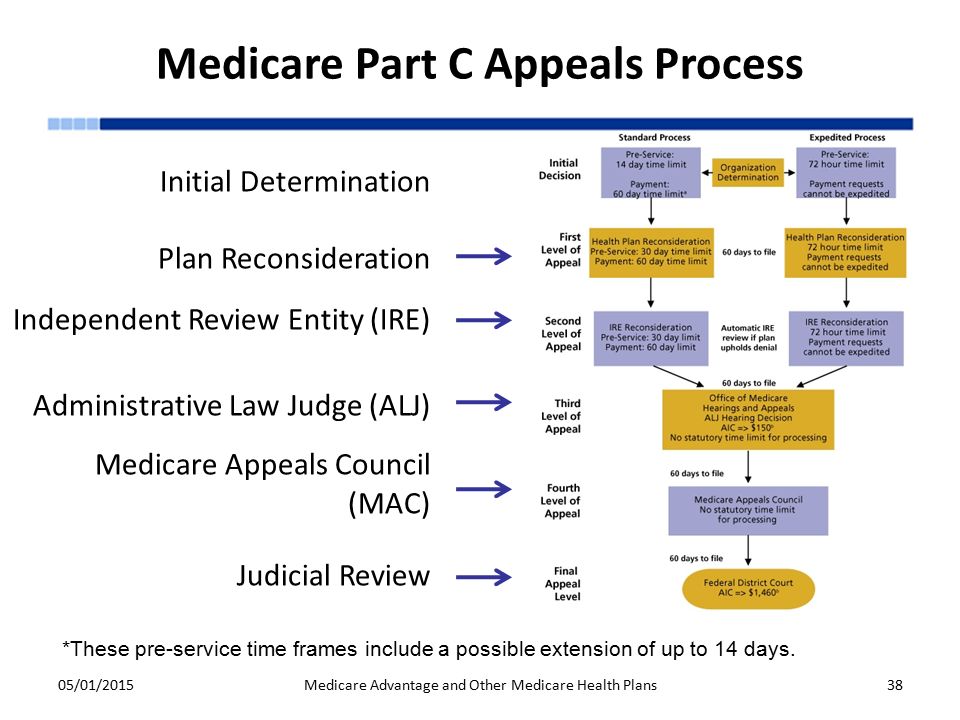
Medicare appeal process diagram. Medicare health plans, which include Medicare Advantage (MA) plans – such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans – Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations. 2.3 APPEAL PROCESS The entire multi-level Medicare managed care complaint process for addressing enrollee challenges to a Medicare managed care adverse organization determination. The IRE reconsideration process is one level in the broader Medicare managed care appeal process. 2.4 DE NOVO REVIEW A review of an individual dispute by a new and ... Claim denials from Medicare, Medicaid and health plans are on the rise, and understanding recent trends in denials is essential to the development of an effective and comprehensive appeal strategy. Among those emerging trends, distinguishing coding denials from clinical validation denials (CVDs) is an ongoing challenge. Medical appeals & grievances process UnitedHealthcare Group Medicare Advantage. The following procedures for appeals and grievances must be followed by your Medicare Advantage health plan in identifying, tracking, resolving and reporting all activity related to an appeal or grievance.
to the Medicare appeals process for Medicare Part A and Medicare Part B (see Pub. L. 106-554). Specifically, Section 521 required, among other features, the establishment of a uniform appeals process for Medicare Part A and Part B appeals, revised time frames for filing appeals and issuing decisions, and the establishment of a new appeal Therefore, understanding the appeals process for Medicare claims is vital for all providers. The aim of this article is to give providers a better understanding of the five (5) levels of the Medicare Appeal process, and what must occur at each level. The Medicare Fee-For-Service (FFS) has five levels in the claims appeal process: The Medicare Appeals Process. The Medicare Appeals Process. fAct Sheet. Overview. Section 1869 of the Social Security Act and 42 C.F.R. Part 405 Subpart I contain the procedures for conducting appeals of claims in Original Medicare (Medicare Part A and Part B). There are five levels in the claims appeals process under Original Medicare: 1. What’s the appeals process for Original Medicare? The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council)
A Medicare Advantage (MA) enrollee also has the right to appeal if the MA plan denies coverage for a service. An MA plan is required to provide enrollees with information regarding the appeals process as part of the plan materials. The appeals procedures for Medicare Part C, including the timeframes for requesting appeals, are different than ... medicare appeals process The third level and beyond Under both the previous and new appeals systems, the third level of appeal is an administrative law judge (ALJ) hearing, and physicians have 60 ... OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If you disagree with a ... • A ll appeal requests must be made in writing. Five Levels in the Appeals Process Medicare offers five levels in the Part A and Part B appeals process. The levels, listed in order, are: • Redetermination by an FI, carrier or MAC • Reconsideration by a QIC • Hearing by an Administrative Law Judge (ALJ) •

The Insurance Approval Process For Proton Radiation Therapy A Significant Barrier To Patient Care International Journal Of Radiation Oncology Biology Physics
New appeal rights are not triggered by a refusal to reopen, and appeal filing timeframes on the original initial determination are not extended following a contractor’s refusal to reopen. See, Pub 100-04 Medicare Claims Processing Manual, chapter 1, §70.5 for the distinction between
Ppt Midwest Home Health Summit Best Practices Conference Series Medicare And Medicaid Audit Defense Appeals From R Powerpoint Presentation Id 1406155
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan. File an appeal. How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Standard Medicare Appeal Letter Templates. Item #: N/A Type: PDF. Download our Standard Medicare appeal letter templates to help you more quickly submit an appeal and ensure you include all necessary information the first time. There is an appeal letter template for each of the five levels of a Standard Medicare appeal process.
— Medicare Appeals Council. If you disagree with the ruling from the previous step, then you can file an appeal to the Medicare Appeals Council. Again, this is the next step regardless of which type of Medicare plan that you have. This council is part of the Department of Health and Human Services (HHS) Appeals Board.
Misalignments in Medicare and Medicaid Appeals Processes The considerable differences between Medicare and Medicaid appeals processes create two distinct paths that Medicare-Medicaid enrollees must navigate when care is denied (Exhibit 1). While new, fully integrated models of care can be designed to offer an aligned appeals process, in most states
The Five Levels of Medicare Appeals . There are five levels in the Medicare appeals process. If at any time your appeal is approved by Medicare, the process ends at the level you are currently on. If a denial is upheld, you will have to decide whether or not to proceed to the next level.
To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals.
Apache Server at www.seniorcitizensguide.com Port 80
The Medicare program includes an appeals system that is broken down into different levels. Steps in the appeals process differ based on whether a beneficiary is enrolled in traditional (original) Medicare, or instead, enrolled in a Medicare Advantage (MA or Part C) plan. Regardless of enrollment, for the most part, appeal
CMS Appeals and Medicare Appeals webpages. Appealing Medicare Decisions Medicare FFS has 5 appeal process levels: Level 1 - MAC. Redetermination. Level 2 - Qualified Independent Contractor (QIC) Reconsideration. Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition. Level 4 - Medicare Appeals Council (Council) Review. Level 5 -

Funding Innovative Dialysis Technology In The United States Home Dialysis And The Esrd Transitional Add On Payment For New And Innovative Equipment And Supplies Tpnies American Journal Of Kidney Diseases
Your Level 1 appeal ("reconsideration") will automatically be forwarded to Level 2 of the appeals process in the following instances: Your plan does not meet the response deadline. If your Medicare Advantage plan fails to meet the established deadlines, it is required to forward your appeal to an independent outside entity for a Level 2 review.
Settled appeals are dismissed Step 10 CMS sends fully executed agreement and Settlement Step 11 Yes Process Over CMS, Appellant & MAC develop consensus Spreadsheet Step 5 Is consensus reached? No Yes Process Complete Low Volume Appeal Settlements Appellant Process Diagram Within 30 days Within 15 days Within 180 days Within 30 days Within 15 ...
The appeals process has five levels. The first level asks Medicare or your Medicare health or prescription drug plan for a "redetermination" on the original request. If your first-level appeal is denied, you may appeal to the next level and the next.
The process of filing a Medicare appeal depends on what type of plan you have. But the appeal process generally has five levels. So, if your original appeal is denied, you will likely have ...
A third level appeal is a bit more interesting as it requires the hearing to be held over the phone, and at times may require a video teleconference; although extremely rare, it may even be in person. Fourth level of appeal . Fourth level appeals are reviewed by the Medicare Appeals Council within the Department of Health & Human Services.
Medicare Hearin gs and A ppeals ALJ Hearing AIC ≥ $180** No statutory time limit for processing . Medicare Appeals Council . No statutory time limit for processing . F. ederal District Court AIC ≥ $ Review1,760** First Appeal . Level Second Appeal Level Third Appeal Level Fourth Appeal Level Judicial
Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review.
Using Matched Survey And Administrative Data To Estimate Eligibility For The Medicare Part D Low Income Subsidy Program















0 Response to "35 medicare appeal process diagram"
Post a Comment